Shoulder osteoarthritis is a widespread chronic disease associated with damage to joint structures. The pathological process is accompanied by degenerative deformation of the articular surfaces. In this case, not only the cartilage tissue is damaged, but also the bone tissue. Symptoms of pathology and methods of treatment depend on the degree of damage to the joints.
The disease can develop over several years without manifesting itself. At some point, under the influence of adverse factors (hypothermia, trauma, severe concomitant disease), the first signs of the disease appear. It is at this time that it is necessary to consult a doctor, since the fight against dystrophic changes in the cartilage is especially effective at the onset of the disease.

Causes of shoulder osteoarthritis
The causes of degenerative-dystrophic damage to the tissues of the joint are many and varied. Among them, injuries play the main role, so post-traumatic arthrosis of the shoulder joint is considered the most common form of pathology. It can be provoked even by slight but repeated damage to cartilage tissue.
In addition, the disease can occur under the influence of the following pathological factors:
- Severe joint damage: synovitis, gout, acute or chronic arthritis, aseptic necrosis of the humerus.
- Regular overstrain of the joints. Most often observed in athletes involved in volleyball, tennis, basketball.
- Congenital pathology of the shoulder joint.
- Endocrine diseases.
- Old and senile age.
- Overweight (obesity).
- Avitaminosis.
- Autoimmune damage and weakening of the immune system.
- genetic predisposition.
Most of the sick are people engaged in monotonous physical labor. Therefore, arthrosis of the right shoulder joint is diagnosed much more often than the left.

The disease usually develops under the influence of not one, but several adverse factors at once. Based on this, treatment should be comprehensive and aimed not only at combating the disease, but also at eliminating all the causes that caused it.
Characteristic signs of the disease
Arthrosis of the shoulder, beginning imperceptibly and developing gradually, can manifest itself suddenly after an injury, hypothermia or heavy physical exertion. In this case, there are characteristic symptoms of damage to the shoulder joints and nearby tissues:
- pain;
- crackles and pops during hand movement;
- stiffness and reduced range of motion in the shoulder.
The disease most often occurs in a chronic form. An exacerbation of the disease can be triggered by excessive stress on the joint or injury.
The intensity of the manifestation of symptoms largely depends on the severity of damage to cartilage and bone tissue, therefore it is customary to distinguish several degrees of the disease. Such systematization significantly facilitates the diagnosis and allows you to accurately predict the outcome of the disease.
Shoulder osteoarthritis I degree
During this period, the tissues of the joint are slightly affected. Pain is observed extremely rarely and only after excessive physical exertion or prolonged monotonous work. The patient most often does not pay attention to these symptoms, attributing them to overwork or muscle fatigue. Defeat of 1 degree is treated only by conservative methods.
At the beginning of the disease, there are no obvious changes in the cartilaginous tissues on x-rays, only an oval ring is noted around the joint cavity.
Shoulder osteoarthritis degree II
At this stage, the symptoms of the disease become more pronounced. Cartilage tissues thin and deform, intra-articular ligaments are damaged. When moving the hand, a crackle is heard, the inner layer of the joint bag inflames. Over time, the pain becomes constant. Morning stiffness and limited movement appear, which can lead to muscle atrophy.

Shoulder osteoarthritis degree III
During this period, the joint is already significantly deformed, there is practically no movement. The patient suffers from sharp pains which can radiate towards the arm and the scapula. If you do not stop the further destruction of tissues, the pathological process can lead to disability.
Third-degree disease is not amenable to conservative treatment and requires surgery.
Shoulder-shoulder arthrosis rarely reaches the third stage. Most often, the second stage is diagnosed with the transition to a chronic form.
Which doctor to contact
Often, people dealing with joint pain do not know where to turn. At the first symptoms of the disease, you should consult a rheumatologist. The specialist will not only conduct a full physical examination and make a diagnosis, but also, if necessary, relieve severe pain with the help of an intra-articular injection of an anesthetic.
With the advanced form of the disease, the rheumatologist risks being helpless. In this case, you will need a surgeon or an orthopedist. In large cities, you can make an appointment with an arthrologist who only deals with joint diseases.
How to Treat Shoulder Arthritis
After a medical examination and diagnosis, the doctor prescribes a specific therapy that allows you to achieve a long and stable remission of the disease. It is impossible to cure degenerative changes in the joints, but to slow down the course of the destructive process and alleviate the patient's condition is quite an achievable task.
The main goal of osteoarthritis treatment is to relieve pain and restore joint mobility.
modern drug therapy
In some patients, it is difficult to make an accurate diagnosis in the early stages of the disease. At this stage, the pain is not pronounced and does not force patients to seek help from specialists. Most often they are independently treated with folk remedies. Some patients engage in therapeutic exercises to reduce joint pain and stiffness. For the treatment of arthrosis, drugs prescribed by a doctor are used, observing the recommended dosage and duration of administration. The most effective are the following groups of drugs:
- nonsteroidal anti-inflammatory drugs;
- chondroprotectors;
- corticosteroid drugs;
- non-narcotic pain relievers;
- vasodilators;
- muscle relaxants.
Many drugs for this pathology are sometimes prescribed for a long time. Depending on the severity of the disease, drugs are taken orally, used externally, injected intramuscularly or into the cavity of the shoulder joint.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs are contraindicated to use for a long time due to the presence of side effects from the digestive tract.
It is possible to treat the disease with drugs already at an early stage in the development of the pathological process. The course is determined depending on the patient's condition and the severity of the symptoms. As an independent treatment, the ointments included in this group are not prescribed. They are used in combination with similar groups of drugs used intramuscularly or orally. Their task is to reduce inflammation and improve the patient's condition.
Chondroprotectors
Almost all patients include drugs aimed at improving metabolic processes in cartilage tissue in the treatment regimen. In addition, they increase the elasticity of the cartilage. Chondroprotectors have such properties. These medicinal substances differ depending on the main active ingredient on the basis of which they are made:
- hyaluronic acid;
- chondroitin sulfate;
- glucosamine;
- combined funds.
Glucosamine is a substance that plays an important role in the formation of healthy cartilage tissue. The job of chondroitin sulfate is to nourish and cushion the shoulder.
Preparations for monotherapy have more proven themselves on the market compared to a combination of substances.
The polysaccharide contained in the intercellular space is hyaluronic acid. It is further able to reduce the sensitivity of receptors that respond to pain. Combined chondroprotectors, which contain several active ingredients, have the greatest advantage.
The most effective use of chondroprotectors in the early stages of the disease. The task of drugs is the synthesis of new cells of healthy cartilage tissue, which replace the damaged tissue. In the presence of pain and swelling, drugs of this group will be less effective. Therefore, it will first be necessary to use anti-inflammatory drugs to alleviate the patient's condition.
To achieve the maximum effect, injection preparations are used for intra-articular or intramuscular administration. The course of treatment with chondroprotectors takes up to six months, some patients notice the first results after 3 months of treatment. It is important to follow certain rules in the treatment of these drugs.
With the start of treatment, physical overload, stressful situations should be excluded. The patient will receive the greatest effect if he starts taking chondroprotectors, improves nutrition and engages in physiotherapy exercises. Many patients with arthrosis of the shoulder joint are engaged in Dr. Bubnovsky's method, they perform a series of specially designed exercises to achieve gradual restoration of the joints or stop the progression of the disease.
Corticosteroid agents
When severe pain appears, if anti-inflammatory drugs do not bring a positive effect, corticosteroids are prescribed. To alleviate the patient's condition, ointments or injections are prescribed.
Painkillers
In the early stages of the disease, painkillers are prescribed to reduce pain.
Compared with nonsteroidal anti-inflammatory drugs, drugs of this group have a less negative effect on the mucous membrane of the digestive tract.
Having an unexpressed anti-inflammatory effect, they effectively fight pain.
Vasodilators
Mandatory means in the treatment of arthrosis are vasodilators. They eliminate vascular spasms, normalize blood flow in the affected area. Many patients complain of the appearance of night pains, which are effectively treated by drugs of this group.
Muscle relaxants
When osteoarthritis of the shoulder joint is affected, muscle spasms are considered a common occurrence, which are relieved by muscle relaxants. When prescribing them, the principle of complexity is observed, they are used with painkillers and anti-inflammatory drugs. If necessary, the minimum dosage is initially prescribed with a gradual increase.
Surgical treatment
The main goal of the operation is to restore the working capacity of the joint and improve the patient's quality of life. If conservative treatment is ineffective, a persistent pain syndrome persists, the joint gradually deforms, and its range of motion is severely limited, the patient is indicated for surgery.
The decision on the need for surgical intervention is made by the orthopedist or traumatologist together with the patient. Next, the dimensions of the stent and the material from which it will be made are determined. Today, implants are made of titanium and high-strength polymers, weighing close to a natural joint. The durability and reliability of stents are beyond doubt.
Recovery period
The operation to replace the affected joint most often takes place without complications. Fixation with a support bandage is necessary for the first 14 days. Early passive performance of a complex of physical exercises on special apparatus and devices is allowed. Electric charges are allowed after 45-60 days.
Physiotherapy
Any complex of anti-arthritic exercises is useful only during remission. If there is an increase in temperature, pain and other symptoms of an exacerbation of the disease, the load is contraindicated.
Exercise therapy should not cause pain or discomfort. At the slightest inconvenience, the exercise must be abandoned.
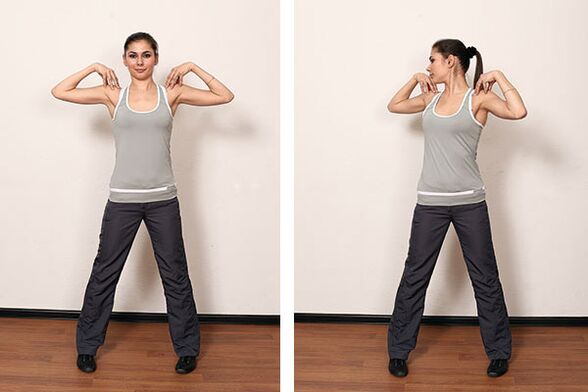
Charging should be done daily. After the load, it is useful to do self-massage in the area of the affected joint and neighboring muscles, using a healing cream, which the attending physician will help you choose.
Physiotherapy
Physiotherapy allows you to increase the effect of drugs, reduce their dosage and minimize the risk of complications. The type of physiotherapy is determined by the doctor, guided by the patient's condition, the neglect of the process and possible contraindications due to concomitant diseases.
Most often, the following physiotherapy procedures are used in treatment:
- magnetic therapy;
- ultrasound with hydrocortisone;
- electrophoresis with anti-inflammatory and analgesic substances;
- ultraviolet radiation
- treatment by laser and infrared rays.
Physiotherapy is carried out in the course of 10-15 sessions several times a year.
Treatment with folk methods
By combining folk remedies with proper drug therapy, exercise therapy, nutrition and physiotherapy, you can achieve a long and stable remission.
One of the best recipes is a compress made from birch leaves, which have anti-inflammatory and warming effects. Young leaves are best suited, since the closer to autumn their beneficial properties decrease. Before making a compress, a small massage of the affected limb is necessary. Then the leaves are applied to the skin, reinforced with cling film and a bandage. The compress is left overnight. The course of treatment is 10 days.
Salt baths have a healing effect. Before the procedure, the crystals are pre-dissolved in warm water. Then the resulting solution is poured into the bath. The procedure will require about 3 kg of salt. Additionally, you can add a few drops of any essential oil. It is better to take a bath before bedtime, the duration of the bath should not exceed 30 minutes.
Hot oatmeal compress helps a lot. They must be poured with boiling water, insisted and used in accordance with their intended purpose. It is recommended to do these procedures at night.
No less useful herbal poultices. Crushed plants with anti-inflammatory action (yarrow, ginger, turmeric, potentilla, calamus) are brewed with boiling water, kept for 10 minutes under a lid and applied to a sore spot. After the procedure, the affected shoulder should be smeared with healing cream and go to bed.
Inside it is recommended to take an infusion of corn stigmas. A teaspoon of raw materials or 1 filter bag is brewed with 200 ml of boiling water, insisted under the lid for 30 minutes and consumed 1 tbsp. spoon half an hour before meals.
Prevention of osteoarthritis of the shoulder joint
Disease prevention can be primary and secondary. Primary prevention includes the following activities:
- regular exercise - jogging or brisk walking, exercises for the muscles of the shoulder girdle;
- cold and hot shower;
- elimination of excessive loads and avoidance of traumatic situations.
- timely treatment of diseases that can cause arthrosis of the shoulder;
Secondary prevention aims at the early diagnosis and treatment of arthritis.
Conclusion
The recovery of joint functions is a long and difficult process. Treatment of arthrosis of the shoulder should be aimed primarily at eliminating the symptoms of the disease. Only complex therapy, combining medical and folk methods, will bring relief and restore working capacity.













































